Author: Alex Neiman
First published: Winter 2023
Course: BMED 530, Dr. Lanny V. Griffin
Institution: California Polytechnic State University, San Luis Obispo
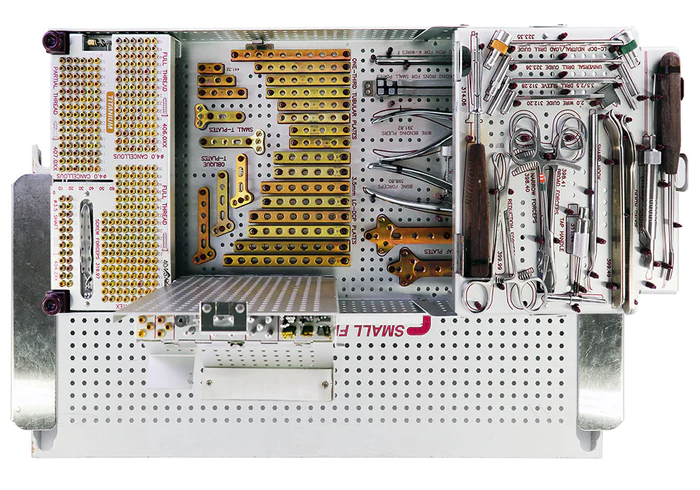 Synthes Small Frag plate set showing screws, plates, and tools commonly used in orthopedic fracture fixation. Source: AA Medical Supply Co.
Synthes Small Frag plate set showing screws, plates, and tools commonly used in orthopedic fracture fixation. Source: AA Medical Supply Co.
Abstract
Contouring, or bending, of fracture fixation plates is a common step in many surgical internal fracture fixation procedures. The necessary precautions for an implant designer include understanding the different types of bending processes that occur and foreseeing the increased risk of fatigue and corrosion due to changes in the microstructure. Strain hardening, galvanic and crevice corrosion, and crack nucleation from plate bending tools should all be carefully considered as part of an implant design. Additionally, a clear understanding of the four major loading scenarios (protection, compression, bridging, and buttressing) and a specific understanding of the fracture site (tibial plateu, acetabulum, etc.) are both required for a robust design.
Introduction
Fracture fixation using plates and screws are a common internal fixation practice in orthopedics. Plates typically have a long service life and may be especially subject to fatigue and corrosion. Due to variation in patient anatomy, plates are commonly contoured intraoperatively to conform to the bone structure. This paper will conduct a comprehensive assessment of the processes, implications, and research available on intraoperative contouring of fracture fixation plates with special consideration to failure and service life . It will also recommend best practices for material selection and design.
Background on fracture fixation plates
Plates are commonly used for a variety of fractures and conditions, specifically during open reduction internal fixation procedures (ORIF). This includes head, trunk, and upper and lower limb fractures. [1]
Locking and non-locking plates
Locking and non-locking plates are the two types of fracture fixation plates. Non-locking plates are traditional devices that require compression between the bone, screw, and plate for loads to be transferred to the plate. Locking screws, in comparison, have a threaded feature in each screw hole that engages directly with the screw, locking the screw orthogonally with the plate and providing a rigid fixation. Locking screws do not require contact or compression between along the screw axis like non-locking plates, so the plates do not need to be tightly contoured to the bone. Locking plates are particularly advantageous in situations where the bone quality is compromised or in fractures near joints, as they do not require bone-to-plate compression and offer improved stability. This paper will primarily consider the case of locking plates, as they make for a more straightforward loading calculation.
Fracture-specific applications
Fracture fixation plates are extremely common in orthopedics. Manufacturers produce large-frag and small-frag sets which can be used as general -purpose sets for a wide variety of bones. Chest fractures are common applications of fracture fixation plates. Rib fractures, especially full nonunions, are treated using long, curved plates. Sternum fractures, including those intentionally occurring during open heart surgery, are fixed with sternum plates. Hand and wrist fractures are another very common application. Fractures of the metacarpals, hamate, and radius are a few examples of small-frag fractures that could be treated by plate fixation. Long bone fractures are also potential applications. Although fractures of the femur, tibia, and other long bones are most commonly treated by intramedullary nailing, fracture fixation plates may be used instead for multifragmentary fractures that would not be well-suited to nailing due to small fragments, spiral fracture, infected bone, or unusual patient anatomy that would not fit a conventional IM nail. Plates may also be used in the long bones to fix fractures at the head or near a joint such as a tibial plateau fracture. Other fracture types could include clavicle, scapula, skull, craniofacial, and pelvic.
Materials
Plates are commonly made from 316L stainless steel, CoCrMo alloys, commercially pure titanium, and other titanium alloys, and are subject to surface finish treatments which may be damaged or removed by bending processes. Although 316L was long the de-facto material for fracture plates, its use has been displaced widely by titanium and its alloys.
Biocompatible alloys
Commercially pure titanium is commonly alloyed with Aluminum, Vanadium, and Niobium to form high-strength materials with improved resistance to galvanic corrosion. To overcome corrosion of Ti, palladium, nickel and molybdenum are sometimes included in the alloy with the drawback of increased material cost. These elements promote cathodic reactions, helping the corrosion system to passivate rather than galvanically corrode. This is, of course, key for biocompatibility, where tissue necrosis due to metal ions is a major concern. However, the inclusion of such elements is expensive.
One key advantage of titanium over stainless steel is the modulus of elasticity which is lower than stainless steel. This can minimize stress shielding and lead to better clinical outcomes. However, although it is reduced, stress shielding is still a concern with Titanium and its alloys- as is any metal. [5, 6]
Although polymeric materials such as PEEK, PMMA, PLA, and PGA have been investigated for use in fracture fixation devices, their poor strength restricts their use to niche applications such as dentistry. Composites of these materials have also been investigated; however, the challenge remains of metal-on-polymer fretting and wear between the screws and the plates. These materials are outside the scope of this paper.
Passivation coatings
Titanium, when exposed to air, naturally forms an oxide layer on the order of nanometers thick. Although this coating itself is corrosion resistant, it is not sufficiently durable to withstand aggressive environments. Anodization processes can increase the oxidation thickness. Additionally, surface treatments could include thermal and chemical oxidative processes and ion implantation. A hydroxyapatite (HA) coating increases corrosion resistance due to the addition of Ca and P ions and the formation of a thicker Ti oxide layer. These thin coatings, when relied upon to provide adequate corrosion resistance, could be inadequate if they are scraped off.
Patient anatomy and contouring
The vast majority of available implants consist of standard size plates. They are mass-produced in standard shapes, with a variety of length options, and are widely considered adequate in terms of clinical outcome. However, the wide variation in patient bone structure requires a bending process to anatomically conform the plate to the bone. Although many modern fracture fixation plates come from the manufacturer in a pre-contoured shape, most plates require some minor modification so that they may conform to the fracture site exactly. [1, 2] The consequences of improper contouring include stress concentration, malreduction, and increased risk of plate or screw failure.
One source performed a comprehensive survey of available designs and illustrated the need for statistical assessment of patient anatomy for implant design. Specifically, the distance from plate to bone ranges from 0.0 mm to 6.0 mm (referred to as the interface distance). This, of course, is highly dependent on the particular application and the type of plate and screw used. Thus, it is quite common for a surgeon to bend the plate intraopreratively, even if they are not designed explicity to be bent (like a reconstruction plate). [3]
Intraoperative bending process
Surgeons use pliers, jaws, presses, and other surgical tools to plastically deform plates during surgery to contour them to the bone [7]. Surgeons may bend the plate multiple times to achieve the most optimal fit, although this is reduced by the inclusion of bendable templates with the frag set. Locking plates have a small-pitch thread in each hole that could be easily deformed by a bending process. Frag kits sometimes include a threaded insert inserted before bending that prevents deformation to the threads. In general, most bending operations can be described as a combination of the following processes. Thinner plates can be bent by hand or may be bent purposefully by a screw during implantation. Other devices, especially thicker, pre-contoured plates, require more serious bending from specialized plate presses.
 Figure 1. Bending a fracture fixation plate out-of-plane using plate irons. Source: AO.
Figure 1. Bending a fracture fixation plate out-of-plane using plate irons. Source: AO.
Out-of-plane bending is commonly performed using hand tools such as bending pliers, plate irons, or plate bender tools as shown in Figure 1. In-plane bending is achieved using the plate irons in Figure 1 or by using plate bending pliers specially designed for in-plane bending as shown in Figure 2. A torquing process involves bending the plate about its axis using plate irons. Tools such as the plate irons would be the most likely to create a scratch or nick on the implant. Bending pliers, on the other hand, are more controlled but bend at a smaller radius. If the surgeon were to use bending pliers, they could risk damage from work-hardening.
 Figure 2. In-plane bending using bending pliers. Source: AO.
Figure 2. In-plane bending using bending pliers. Source: AO.
Plate bending can also be performed with a plate press. This is a large, hand operated, compound lever tool used for bending thick plates. The plate press, due to its compounding lever action, has the potential to apply a critical stress to a plate, so it especially has potential to create undesirable mechanical defects.
 Figure 3. Zimmer Plate Bending Press 100.06.010. Source: Zimmer Biomet
Figure 3. Zimmer Plate Bending Press 100.06.010. Source: Zimmer Biomet
At times, the correct size plate is not available, so surgeons must shorten plates by cutting them. In some cases they use a specialized plate shear. Other times they may resort to using pin cutters or other general cutting tools. Any cutting tool will expose the inside plate material. Although it likely has time to oxidize inside the operating room prior to implantation (to form a passivation layer in the case of Titanium), this would nullify any specialty passivation coating applied by the manufacturer and may compromise the corrosion resistance of the device.
Loading conditions
Loading conditions for plates includes protection (neutralization), compression, bridging, and buttressing (antiglide), each having unique loading conditions. The loading conditions for a plate could be as high as the service load of the bone itself, plus any additional stresses imparted by screws, etc. The service loads for a device such as a single lateral plate for femur fracture could range from the 10 Pa to the 100 kPa (von Mises stress) [3], with a maximum potentially in the 10 MPa range in the case of a fully supported bridging scenario of cross sectional area of 30 mm^2^ with an 80 kg patient. Another literature review reported the daily load on a plate to be between 0.5% and 400% of a patient’s body weight for full weight-bearing conditions.
Protection (neutralization)
Orthopedists use plates to protect another fixation, commonly a single lag screw. This screw would bear the majority of the compressive force for the fixation. The objective is to reduce the degrees of freedom to prevent bending and rotation of bone fragments; more specifically, it is to restrict the rotational motion of the bone about the axis of the lag screw. This loading case would not see axial loading of the plate but instead in-plane shear.
Compression
Plates can be used like a spring to compress a nonunion after it has been stabilized. The plate is plastically deformed into a curved shape before it is implanted, and it is then elastically deformed by tightening the plate straight against the bone using screws. This spring-like behavior keeps the nonunion under compression, allowing it to heal. This loading case would see minor flexile stresses due to the spring behavior. It is not expected to see severe loading in the axial direction. Also worth mentioning is that non-locking plates are used for compression-mode applications; the screws are not attatched perpendicular to the plate face, so loading conditions differ due to the non-locking screws as well.
Bridging
Bridging is a technique for multifragmentary long bone fractures where fixation of individual bone fragments or fixation at the site of the fracture is not well-suited. A long plate provides relative stability by setting the correct alignment of the two bones on either side of the fracture, leaving the fracture site alone to heal. This loading scenario is the most rigorous, having to bear as much load as required to support the bone without major stress shielding. In this case, patients would be advised to reduce weight bearing until the fracture has healed, which would be a longer time than would be prescribed for an IM nail fixation. Under these conditions, a fracture plate would see major compressive loading, plus torsion and flexure stresses as would be encountered in the bone. This would be the closest of these four cases to axial loading, although it would be truly far from it.
Buttressing (antiglide)
Similar to the protection case, the buttressing technique entails supplementing a lag screw fixation. In this case, the goal is to reduce the shear stresses on a screw by supporting the fracture with a curved plate. In this case, the screw likely bears the majority of the total service load, but the plate would still see out-of-plane shear and flexure stresses.
Failure
Plates may fail during their long service life, which may range from one or two years up to indefinitely. Due to the cyclic loading conditions commonly encountered in orthopedic applications, plate devices are expected to have a high fatigue resistance and preferably have a low modulus of elasticity to minimize stress shielding.
The typical modes of failure for fracture fixation plates are those related to corrosion-fatigue [4]. Even highly corrosion resistant alloys such as commercially pure titanium and other Ti alloys are susceptible to corrosion-induced failure.
Of particular concern is the early failure of plates due to nucleation sites created by damage during surgery. These can be caused by the commonly-referred-to “surgical error”; however, this paper aims to investigate whether routine bending operations could induce similar fatigue failures. These nicks or scrapes can act as nucleation sites for cracks which would cause catastrophic failure of the device.
At a material level, other causes of failure outside the scope of this paper are embrittlement due to alloy sensitization and inclusions of impurities, both of which are also likely reasons for fracture fixation plate failure.
Effects of plate bending on fatigue resistance
Even though plate contouring is common practice, the available literature on mechanical properties of devices after bending is sparse. There have been several studies attempting to quantify the effects of bending on fatigue resistance, one of which involving fatigue testing on plates bent up to 9 times repeatedly. It is likely that such research is proprietary and internal to the implant engineering companies. What is clear, however, is that implants are designed to be [1]. The addition of relief features into the side of plates lowers the moment of inertia in the non-screw-hole locations, allowing a more uniform bend and protecting the threads in the screw holes.
One study performed fatigue testing on three different series of Stryker stainless steel (SS) 316LVM fracture fixation plates with lengths around 4 inches. They performed a 20º bend in the plate with a plate bender on various samples between one and nine times in the same location. They then performed a cyclic fatigue test and compared the results. One plate system showed no significant difference in fatigue, while one system was shown to have significantly lower fatigue strength. Interestingly enough, the third system showed an increase in fatigue resistance in the plates that were bent with three repititions. This could be an intraoperative work-hardening process expected and accounted for by the implant manufacturer [8]. To be noted is that this test was performed in air and did not account for any corrosion-induced fatigue failures.
Surgeons are aware of the implications of plate contouring on implant fatigue strength and are advised to make their bends in the parts of the plate that do not see the maximum strain. It is up to the surgeon to use plates appropriately, apply the mechanics of fracture healing, and advise their patients appropriately on weight-bearing procedure to reduce the probability of a fatigue induced failure. [9]
Bibliography
[1] H. Uhthoff, P. Poitras and D. Backman, “Internal plate fixation of fractures: short history and recent developments,” Journal of Orthopedic Science, vol. 11, p. 118, 2006.
[2] Y. Bai, Y. Deng, Y. Zheng, Y. Li, R. Zhang, Y. Lv, Q. Zhao and S. Wei, “Characterization, corrosion behavior, cellular response and in vivo bone tissue compatibility of titanium–niobium alloy with low Young’s modulus,” Materials Science and Engineering, vol. 59, p. 565, 2015.
[3] P. D, B. A and D. MV, “Corrosion of Titanium: Part 1: Aggressive Environments and Main Forms of Degradation,” Journal of Applied Biomaterials & Functional Materials, vol. 15, p. 291, 2017.
[4] S. G. B. d. Koning, N. d. Winter, V. Moosabeiki, M. J. Mirzaali, A. Berenschot and M. M. E. H. Witbreuk, “Design considerations for patient-specific bone fixation plates: a literature review,” Medical & Biological Engineering & Computing, 2023.
[5] E. E. III and W. Schubert, “Plate bending Basic techniques,” AO, [Online]. Available: https://surgeryreference.aofoundation.org/cmf/basic-technique/plate-bending.
[6] G. S. Lewis, D. Mischler, H. Wee, J. S. Reid and P. Varga, “Finite Element Analysis of Fracture Fixation,” Curr Osteoporos, vol. 19, no. 4, pp. 403-416, 2021.
[7] C. Kanchanomai, V. Phiphobmongkol and P. Muanjan, “Fatigue failure of an orthopedic implant – A locking compression plate,” Engineering Failure Analysis, vol. 15, no. 5, p. 521, 2008.
[8] J. A. Bishop, S. T. Campbell, M. L. Graves and M. J. Gardner, “Contouring Plates in Fracture Surgery: Indications and Pitfalls,” Injury, vol. 28, no. 14, p. 585, 2020.
[9] A. Lin, C. Fechter and M. Magill, “The effect of contouring on fatigue resistance of three types of fracture fixation plates,” Journal of Orthopedic Surgery and Research, vol. 11, 2016.
[10] W. M. Ricci, “Risk Factors for Failure of Locked Plate Fixation of Distal Femur Fractures: An Analysis of 335 Cases,” Journal of Orthopaedic Trauma, vol. 28, no. 2, p. 83, 2014.
[11] S. Zhang, D. Patel and M. Brady, “Experimental testing of fracture fixation plates: A review.,” Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine. , vol. 236, no. 9, pp. 1253-1272, 2022.